Stem Cell Therapy
- Home
- CELLAAX Therapy
- Stem Cell Therapy
STEM CELLS THERAPY
MSC Therapy
What are mesenchymal stem cells (MSCs)?
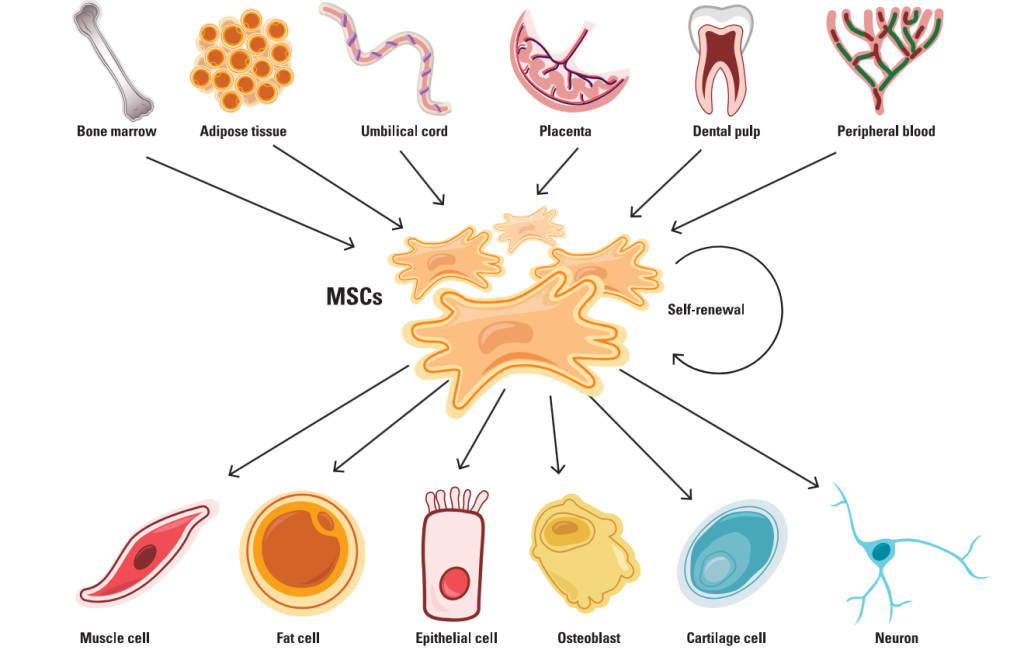
In the 1960s and 1970s, Alexander Friedenstein, a histologist at the USSR Academy of Medical Sciences, isolated a unique type of stromal cells from the bone marrow of mice. When cultured in vitro and transplanted in animals, these spindle-shaped cells differentiated into bone, cartilage, and fat cells (1). This observation led to the discovery of MSCs. Later, scientists found that while MSCs are primarily present in bone marrow, they also reside in other tissues, such as fat, the umbilical cord, peripheral blood, and the dental pulp (2).
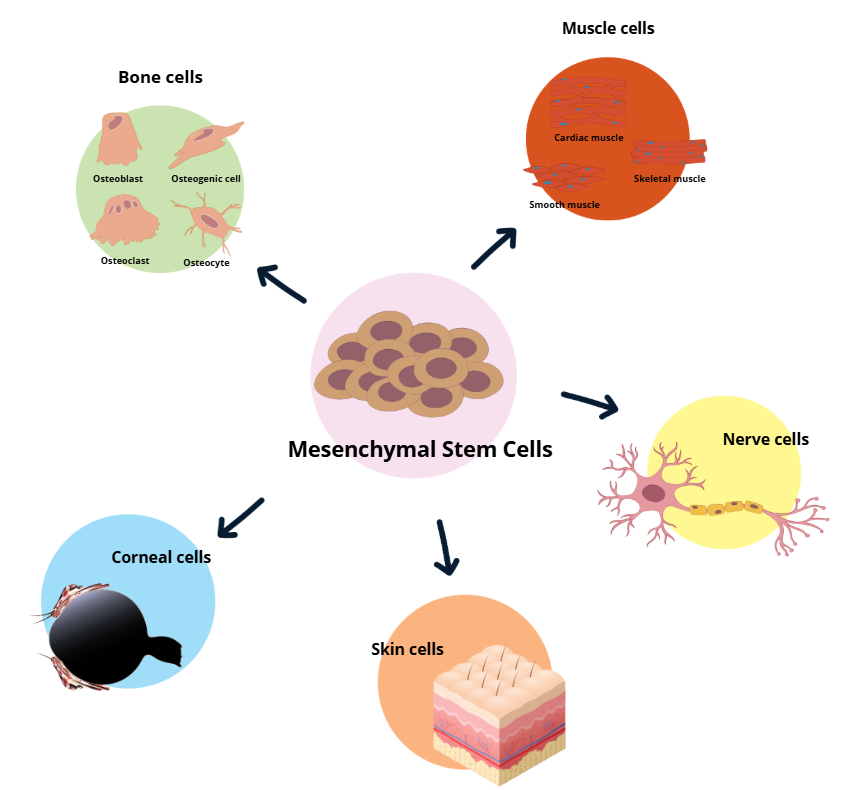
Unlike embryonic stem cells, which can develop into any cell type in the body, MSCs are multipotent. This means they can differentiate into a selected range of cell types, including epithelial cells, muscle cells, neurons, and connective tissues like bone, cartilage, and fat (2). MSCs possess self-renewal capabilities, allowing them to replicate and maintain their population over extended periods and supporting ongoing tissue regeneration.
Beyond their self-renewal and differentiation potential, MSCs play a crucial role in modulating immune responses, particularly in inflammatory environments such as infections or wounds. For example, when inflammation occurs, MSCs migrate to the affected tissues, where they aid in tissue repair by releasing specific cytokines and mediators that inhibit effector T cells’ activity and activate immune-suppressing regulatory T cells, restoring immune homeostasis. Additionally, MSCs exhibit antifibrotic properties by remodeling the extracellular matrix and reducing myofibroblast activity. They also secret pro-angiogenic factors that promote the formation of new blood vessels (3).
Our advanced protocols are backed and proven by science to treat a myriad of conditions. Find out more on how our MSCs can help your condition by reaching out to us today.
What are mesenchymal stem cells (MSCs)?
The various sources from which MSCs can be isolated, their ability to differentiate into diverse cell types, and their immunological properties make MSCs attractive therapeutic tools. Regulatory agencies worldwide have approved twelve MSC-based therapies, and over 1,000 clinical trials have been conducted or are underway to explore their potential in treating a wide range of diseases (4).
In bone regeneration, MSCs present a promising alternative to traditional autogenous bone grafts, which have limitations such as unpredictable absorption, prolonged recovery time, and pain at the harvest site. Clinical studies have shown that bone marrow- and umbilical cord-derived MSCs can improve healing in bone fractures and alleviate pain in osteoarthritis (5,6). In wound healing, MSCs have shown efficacy in enhancing tissue regeneration and reducing scarring by promoting fibroblast and endothelial cell growth. Several clinical trials have reported successful results in healing chronic wounds, ulcers, and vocal fold scarring with minimal severe side effects (7,8).
Meanwhile, scientists are investigating MSCs’ role in treating neurological disorders such as amyotrophic lateral sclerosis, Parkinson’s disease, and stroke (9–11). In these diseases, MSCs may help repair damaged motor neurons and improve functional recovery. Cardiovascular diseases also benefit from MSC therapies, with studies showing that transplanting MSCs to patients with myocardial infarction elevates myocardial viability and heart blood flow (12). Additionally, MSCs’ have been tested in treating autoimmune diseases, such as rheumatoid arthritis and type 1 diabetes, where they may modulate overactive immune responses, and cancer, where genetically modified MSCs could target tumor sites and deliver anti-tumor agents (13,14).
How do MSCs exert their therapeutic effects in the body?
Following administration, MSCs travel through the bloodstream and react to inflammatory signals such as chemokines released by the damaged tissue. These chemokines create a gradient that directs MSCs toward the injury site and prompts the endothelial cells lining the blood vessels to express adhesion molecules on their surfaces. As MSCs flow by, they roll along the endothelial surface and latch on these adhesion molecules via their surface receptors like integrins. Once securely adhered, MSCs squeeze through the endothelial barrier and continue to follow the chemical signals to reach the injury site (15). Once there, MSCs adapt to the local microenvironment and differentiate into the cell types needed to repair the injury.
In addition to directly turning into specialized cell types, MSCs play their therapeutic role through paracrine signaling by secreting a wide array of bioactive molecules, including cytokines, growth factors, and extracellular vesicles containing messenger RNAs, microRNAs, and peptides. These paracrine factors modulate the local microenvironment, promoting cell survival, proliferation, and tissue regeneration. For example, MSCs release vascular endothelial growth factor (VEGF), which facilitates angiogenesis, the formation of new blood vessels essential for supplying nutrients and oxygen to damaged tissues. They also secrete antiapoptotic factors such as hepatocyte growth factor, interleukin-6 (IL-6), and miRNA-25 to enhance cell survival, and antifibrotic factors like prostaglandin E2 (PGE2) and IL-10, which help reduce fibrotic scarring (16).
Another key mechanism by which MSCs exert therapeutic effects is immunomodulation through a combination of secreted factors and direct cell-to-cell interactions. They secrete anti-inflammatory molecules such as transforming growth factor beta (TGFβ), PGE2, IL-10, and indoleamine 2,3-dioxygenase (IDO), which suppress the activity of T cells, B cells, dendritic cells, and natural killer (NK) cells. MSCs also influence the immune system through direct contact by expressing surface molecules like programmed death-ligand 1, which induces T cell apoptosis and promotes regulatory T cell development. Additionally, MSCs can shift macrophages from a proinflammatory state to an anti-inflammatory state (17). By limiting inflammation, MSCs create an immunosuppressive environment for tissue to heal and regenerate.
Mesenchymal Stem Cells (MSCs)
Mesenchymal stem cells are adult stem cells isolated from different sources that can differentiate into other types of cells. In humans, these sources include; bone marrow, fat tissue, umbilical cord tissue (Wharton’s Jelly) or amniotic fluid (the fluid surrounding a fetus).
Mesenchymal stem cells (MSCs) can differentiate into many different types of cells within the body, including:
Why CELLAAX MSCs?

SAFETY
Well tolerated by patients in clinical trials. Our MSCs are manufactured and administered according to cGMP CGTPs standards with refined procedure which comply to the highest health and safety standards.

SUPERIORITY
We aim to provide effective and superior quality cells. Our MSCs are healthy cells with high viability fulfilling all QA and QC stringent validation adhering to international regulatory standards.

EFFECTIVENESS
Our effective MSCs comply three major factors:
1. Multilineage differentiation potential.
2. Immunomodulatory properties that restore immune regulation.
3. Paracrine effects which promote tissue repair and cell proliferation.
Treatable Diseases using CELLAAX MSCs
We are harnessing the power of Regenerative Medicine to bring cutting edge
treatments that can heal and cure.

Ocular
Retinitis Pigmentosa

Neurological
Autism Ataxia Alzheimer’s Disease Cerebral Palsy
Cardiovascular
Stroke
Heart Attack

Wellness
Anti-Aging Skin Rejuvenation Wounds Care
Infertility
Premature Ovarian Failure Erectile Dysfunction

Other Diseases
Autoimmune Diseases Orthopedic Post-COVID Rehabilation
